Mission
Neurology Networks tries to offer broad exposure to various topics that may be presented on the veterinary neurology board exam.
Hepatic encephalopathy
"Hepatic encephalopathy: etiology, pathogenesis, and clinical signs."
Salgado M, Cortes Y.
Compend Contin Educ Vet. 2013 Jun;35(6):E1-8
Hepatic encephalopathy is altered mentation related to neuronal inhibition from accumulation of hepatic toxins/ byproducts. There are four encephalopathic stages (See table).

Ammonia hypothesis – basis for most theories of pathogenesis of HE. States that most signs are related to complications from accumulation of ammonia in the brain. Astrocytes in the brain will convert ammonia to glutamine in normal conditions by glutamine synthetase. Glutamine is extruded from the astrocytes and taken up by nerve terminals for conversion to glutamate for neurotransmission.
In hyperammonemia, glutamine forms, but release from astrocytes is inhibited. The cells therefore swell from cellular edema (glutamine is osmotically active).
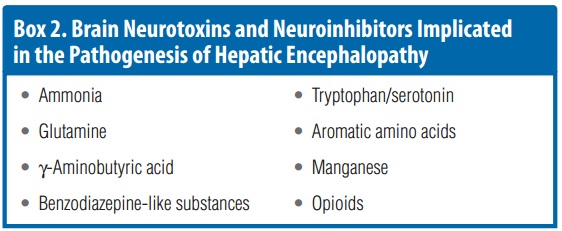
**Blood ammonia levels don’t always correlate to clinical signs so there is probably more than just ammonia involved. Several toxins are implicated including those in the following table:
Inflammation concurrent with hyperammonemia makes neuro signs worse, so inflammatory mediators may also be involved. Ibuprofen helped a rat model of HE suggesting inflammation plays a significant role.
A lot of factors can lead to hyperexcitability and therefore seizures (impaired chloride extrusion, suppressed inhibitory neurons, glutamate-mediated neuronal depolarization, etc).
Oppositely excess GABA activation can exacerbate obtundation. It can also increase GABA sensitivity to benzodiazepine compounds, making HE patients more prone to side effects from these drugs. This is improved in some models with use of Flumazenil (benzodiazepine inhibitor).
Serotinin, serotonin receptors, and monoamine oxidase inhibitors are increased in humans with HE.
Aromatic amino acids reduce catecholamine activation. This combined with reduced dopamine production lead to reduced brain activation.
HE leads to increased manganese in the blood which contributes to Altzheimers astrocytosis.
Other potential neurotoxins: taurine, opiods, melatonin, methanthiols, short-chain fatty acids. Support for the active contribution to HE is inconsistent.
** Ultimately HE is a complex biochemical process that can include several types of transmitters and can therefore show signs despite having normal ammonia levels. Treatment is not straightforward and includes supportive care, careful use of benzodiazepines and drugs metabolized by the liver, and possibly anti-inflammatories, etc.
